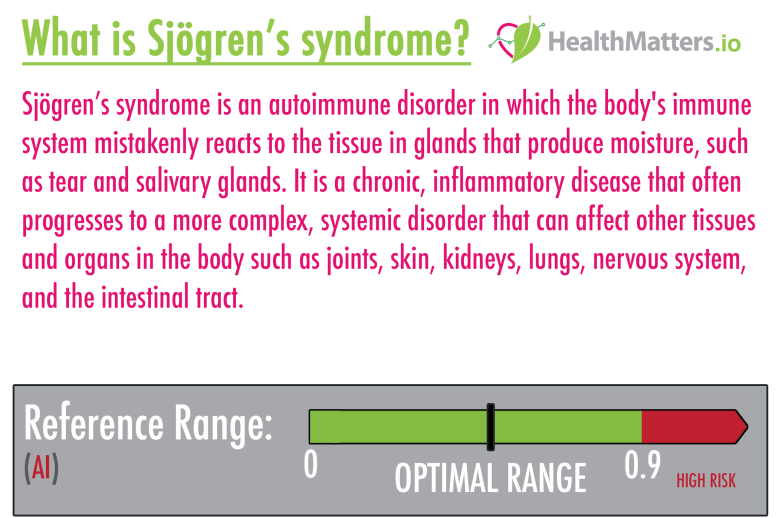
- Sjögren’s syndrome is an autoimmune disorder in which the body’s immune system mistakenly reacts to the tissue in glands that produce moisture, such as tear and salivary glands.
- It is a chronic, inflammatory disease that often progresses to a more complex, systemic disorder that can affect other tissues and organs in the body such as joints, skin, kidneys, lungs, nervous system, and the intestinal tract.
- Sjögren’s syndrome is characterized by an unusual accumulation (infiltration) of a particular type of white blood cell, lymphocytes, in the glands that are responsible for fluid production.
- Pregnant women who have autoantibodies related to Sjögren’s syndrome may have a higher risk of miscarriage.
- Sjögren’s syndrome has also been associated with a higher risk of developing lymphoma.
- Sjögren’s syndrome may present as primary or secondary disease, with all cases divided roughly in half between the two:
- Primary Sjögren’s syndrome develops gradually with salivary and tear gland function worsening over time and without any other underlying disorder. Primary Sjögren’s syndrome has a strong female propensity and is more prevalent in Caucasian women, with the mean age of onset usually in the 40s.
- Secondary Sjögren’s syndrome occurs when a person already has an autoimmune disorder, such as lupus, polymyositis, scleroderma, or rheumatoid arthritis.
- Complications can may include salivary gland infections and tumors, dental cavities, damage to the eyes, kidney disease, and lung infections.
What is the cause of Sjögren’s syndrome?
The cause is not known, but it may be a combination of genetic and environmental factors. It is thought that a trigger such as a bacterial or viral infection may prompt development of Sjögren’s syndrome in some people who are genetically predisposed to the disorder.
What are the symptoms?
Diagnosing Sjögren’s syndrome can be challenging as they vary from person to person and change in type and severity over time. Many people with Sjögren’s are able to live normal lives.
Here is a list of possible symptoms:
-
- Chronic fatigue
- Chronic fever
- Decreased sense of taste and smell
- “Sicca syndrome“
- Dry gritty eyes
- Dry mouth with difficulty swallowing or talking
- Dry skin and rashes
- Dry cough
- Fatigue
- Joint pain and swelling
- Muscle pain
- Numbness or tingling in the hands or feet
- Sore tongue or throat
- Swollen salivary glands
- Vaginal dryness
- Stomach upset, irritable bowel
- Recurrent bronchitis or pneumonia
The epidemiology of Sjögren’s syndrome:
- According to the National Institute of Neurological Disorders and Stroke (NINDS), between 1 and 4 million people in the United States have Sjögren’s syndrome.
- Sjögren’s syndrome can affect anyone at any age, but the majority of those afflicted are older than 40, and women are nine times more likely than men to have the disorder.
- It is estimated to be the second most common autoimmune disease, after lupus.
Testing and diagnosing Sjögren’s syndrome:
- Testing for Sjögren’s syndrome includes looking at symptoms and performing the following tests:
anti-SSA antibodies are often found together with anti-SSB. However, anti-SSA antibodies alone are often found in lupus, particularly in limited forms of the disease. anti-SSA often appears before anti-SSB.
Interpretation:
- Anti-SSA levels may be elevated in the following conditions:
- Sjögren’s syndrome: 60%-70% of cases
- Systemic lupus erythematous (SLE): 25% of cases
- Both anti-SSA and Anti-SSA are usually absent in secondary Sjögren’s syndrome.
- When anti-SSA levels are elevated in SLE, it is often in antinuclear antibody (ANA) – negative lupus.
- Anti-SSA plus anti-La/SSB is associated with the following factors:
- Age older than 50 years
- HLA-DR3
- Lower likelihood of anti-DNA antibodies
- Anti-SSA without anti-La/SSB is associated with the following factors:
- Age younger than 22 years
- HLA-DR2
- Worse renal manifestations
- Increased likelihood of anti-DNA antibodies
- Sjögren’s antibodies (SS-B) is detected in approximately 15% of patients with Sjögren’s Syndrome. Sjögren’s antibody (SS-B) is present only if Sjögren’s antibody (SS-A) is also detected. The presence of both antibodies (SS-A and SS-B) strengthen the diagnosis of Sjögren’s Syndrome and conveys prognostic information.
- Anti-Ro antibodies are found in 60 to 90% of patients with Primary Sjögren’s syndrome and 30 to 40% of patients with SLE who appear to fall into specific subsets.
Possible treatment:
Most of the treatment for Sjögren’s syndrome is aimed at relieving symptoms of dry eyes and mouth and preventing and treating long-term complications such as infection and dental disease. Treatments often do not completely eliminate the symptoms of dryness.
Clinical references:
- Clinical utility of common serum rheumatologic tests. [L]
- Reviewing primary Sjögren’s syndrome: beyond the dryness – From pathophysiology to diagnosis and treatment. [L]
- Sjögren’s syndrome: Clinical aspects. [L]
- Sjögren’s syndrome. [L]
- Biomarkers for Primary Sjögren’s Syndrome. [L]
- Sjögren’s syndrome: a forty-year scientific journey. [L]
- The epidemiology of Sjögren’s syndrome [L]
- Autoantibodies in Sjögren’s Syndrome [L]
- Genes and Sjögren’s Syndrome [L]
- In primary Sjögren’s syndrome, HLA class II is associated exclusively with autoantibody production and spreading of the autoimmune response. [L]
Disclaimer:
The information on healthmatters.io is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.

Do you know why this disease affects women more than men?
Hi @aboutepilating :)! The short answer is that it could be because of declining hormonal levels related to menopause.
Here’s more info on this:
“Although Sjögren’s syndrome can occur in women during child-bearing years, most cases of SS occur soon after menopause around age 55–60. Clinical and animal model evidence indicates that estrogen and androgens like DHEA promote gland cell survival and protect against exocrine gland inflammation; and these hormone levels decline at menopause. Even though estrogen levels drop significantly prior to menopause and androgens gradually decrease, low levels of estrogen continue to drive autoantibody diversity. Other female-dominate rheumatic ADs like SLE and RA increase the risk of developing SS and generate similar autoantibody profiles. Extraglandular manifestations of SS follow typical sex difference predominance with thyroiditis, Raynaud’s phenomenon, depression, and fibromyalgia occurring more frequently in women than men, while lymphoma occurs more frequently in men. Overall, estrogen may increase the incidence of SS in women by increasing autoantibody production, even following menopause, leading to IC deposition, tissue damage, TLR/ inflammasome activation, elevated IFNs, and exocrine gland dysfunction. Importantly, sex hormones most likely contribute to SS pathology in the context of genetic predisposition and environmental triggers like infections.”
Sex differences in Sjögren’s syndrome: a comprehensive review of immune mechanisms (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4630965/)
I hope this help!
Have a great day!
Thank you for the feedback and for taking the time to respond.